Connect With Us

Bunions
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
Blisters Between the Toes

Blisters between the toes can be painful and uncomfortable, often causing irritation with every step. The primary symptom is a fluid-filled bump that forms between the toes, which may be red, swollen, or tender to the touch. Blisters are typically caused by friction, such as from wearing poorly fitted shoes or excessive moisture. Activities like running or dancing can also increase the risk of developing blisters in this sensitive area. The friction can lead to a burning or stinging sensation, especially when pressure is applied. Popping a blister yourself is not recommended, as it can lead to infection. A podiatrist can help by properly draining any painful blisters and providing advice on prevention, including recommending the right footwear, moisture-wicking socks, or custom orthotics. This type of doctor may also offer guidance on how to care for the area to avoid infection and encourage faster healing. If you have developed blisters between the toes, it is suggested that you schedule an appointment with a podiatrist.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact Patricia Mcilrath, DPM of Health One Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact our offices located in Reading and Rittenhouse, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters
Blisters are small pockets of fluid that occur on the top layers of the skin for several reasons. Friction, burns, and diseases are all known causes of blisters. Smaller blisters are known as vesicles, while larger blisters are referred to as bulla. The fluid inside the bubble can be blood, pus, or serum; which is a clear liquid that protects the skin. In most cases, blisters are not a major health issue, but they can be an indicator of a more serious condition.
Causes of blisters vary. Blisters are commonly caused by wearing poorly fitted shoes that rub against the foot. However, there are many other causes besides from friction; including burns, sunburn, insect bites, frostbite, poison ivy/oak, chemical exposure, impetigo, eczema, viral infections, and more.
Most blisters heal by themselves and do not require immediate medical care. If you have a blister, do not pop it since this may cause infection; it is advised to put a bandage over the blister to protect it. If the blister is large, causes pain, or if you have a fever, it is recommended that you see a doctor who can provide proper care. Blisters are easy to diagnose, and if considered prudent by the doctor, can easily be drained of fluid with a sterile needle as well.
To prevent blisters on the feet, wear shoes that fit properly and don’t cause rubbing. Socks can help prevent friction and it is recommended that you wear them if you are wearing shoes. Hand blisters can be avoided by wearing gloves during activities that cause friction against the hand. If you have a blister that pops, do not remove the dead skin, wash the area, apply antibiotic ointment, and cover with a bandage. It is okay in most cases to not seek immediate medical care for a blister if it was just caused by friction. However, if the blister causes pain or does not go away, it is suggested that you see a doctor for a diagnosis.
How Gait Disorders in Seniors Impact Their Feet

Gait disorders in the elderly significantly affect the feet, leading to discomfort, instability, and a higher risk of falls. These conditions often result from musculoskeletal issues, neurological disorders, or chronic diseases, such as arthritis and diabetes. Weakness in the foot muscles, joint stiffness, and loss of sensation contribute to unsteady movement, increasing the likelihood of injuries. Pain and deformities like bunions or hammertoes further disrupt balance, making walking difficult. Reduced mobility leads to a loss of freedom and independence, affecting mental well-being and overall quality of life. Fear of falling may cause seniors to limit their activities, resulting in muscle weakness and further instability. If you are elderly or caring for an elderly individual and notice a change in the feet or walking patterns, it is suggested that you consult a podiatrist who can offer corrective treatment and proper foot health guidance.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact Patricia Mcilrath, DPM from Health One Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our offices located in Reading and Rittenhouse, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Taking Care of Elderly Feet
Many foot diseases and conditions become more serious and common among the elderly. Some of these conditions include diabetic ulcers, ingrown toenails, fungus, arthritis, corns, and calluses. Unfortunately, it may be harder for older adults to take care of their own feet, but there are some precautions they can take in order to avoid any serious conditions.
Dry, cracked heels tend to be a common problem for older people. In order to avoid this, you should always keep your feet clean and well moisturized. Special feet moisturizers should be used as average lotions might not provide enough moisture for dry and cracked heels. Daily foot inspections are crucial for the elderly to detect any irregularities in their earliest stages. During the aging process, blood circulation tends to slow down causing older people to not feel their feet as well as they used to. This often results in foot problems going unnoticed.
Fungal and bacterial conditions thrive on elderly feet because older adults are less likely to keep their feet clean and dry; this makes it easier for bacteria to take hold in their dry, cracked skin. Elderly people should be sure to thoroughly dry their feet, especially in between the toes, after bathing. This will help them avoid developing any fungal infections. Additionally, clean cotton socks should be worn after the feet are dried.
Cutting toenails straight across will help prevent ingrown toenails. When toenails are cut too lose, the nail might break through the skin resulting in an ingrown nail. Clippers should be used to cut the nails in order to make the cut even.
Elderly people who have diabetes are at risk of developing serious foot problems that may lead to amputation. Ulcers that are left untreated can lead to gangrene. Dry and cracked feet, fungus, and untended cuts under the nails may also lead to infections.
Fortunately, Medicare covers many different types of services for foot care. Elderly people with any of these foot conditions should seek the help of a podiatrist and perform daily foot inspections in order to ensure that they have healthy feet.
Choosing the Right Running Shoe for Your Foot Type
Running may seem like a simple to do. However, running is actually a complex movement that puts stress on the ligaments, bones, and joints of the body. Selecting the correct running shoe is important for increasing performance and avoiding risk of injury. Running shoes should be selected based on your foot type. Considerations such as trail versus road shoes are important. Your foot type dictates the degree of cushioning, stability and motion control you require. The most accurate way to learn your foot type is to visit a local shop that specializes in running shoes. Professionals can measure your arch type, stride and gait and help you with your shoe needs.
The design of running shoes is created around the idea of pronation. Pronation is the natural rolling movement of your ankle from the outside to inside when your foot strikes the ground. If you run properly you strike the ground on the outside of your heel and roll in the direction of your big toe before pushing off once more. Pronation is beneficial because it assists the lower half of your body in absorbing shock and storing energy. Those considered neutral runners pronate correctly and do not need running shoes that help correct their form. Neutral runners can choose from a wide variety of shoes, including barefoot or minimal types. However, those who have arch problems or who adopt an incorrect form while running may experience too much or too little pronation. They may require running shoes that offer additional support.
Those who overpronate experience an over-abundance of ankle rolling. Even while standing, those who severely overpronate display ankles that are angled inward. It is not uncommon for them to have flat feet or curved legs. The tendency to overpronate may cause many injuries. Areas that tend to become injured are the knees, ankles, and Achilles tendon. If you find that you have a tendency to overpronate, you should look at shoes that provide extra stability and motion-control. Motion-control shoes are straight and firm. Shoes of this type do not curve at the tip. The restricted flexibility along the middle of the shoe prohibits the foot from rolling too far inward as your foot strikes the ground.
A less common problem is underpronation. Underpronation, also called supination, is when the feet are unable to roll inward during landing. Those who underpronate have feet that lack flexibility and high arches. This prevents any kind of shock absorption, even though it does place less rotational stress on ankles and knees. This added force can cause fractures, ligament tears, and muscle strains because the legs are trying to compensate for the impact. Those who underpronate need shoes with more cushioning and flexibility. If you have a tendency to underpronate, selecting stability or motion-control shoes may cause you more problems by continuing to prevent pronation.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
How Obesity Affects Your Feet
Gaining weight can happen suddenly and at any time. Usually you won’t notice the extra weight until your feet start hurting at the end of the day. This happens as your feet begin adjusting to carrying more weight. Foot swelling and pain are two of the biggest side effects of having gained weight.
Many foot-related problems can occur even after just putting on a few pounds. This includes the body ‘compensating’ by changing the way it moves. You may find yourself putting extra weight on the wrong parts of your feet and even leaning forward a bit. Your feet were designed to carry a healthy, normal body weight. Extra weight places undue stress on them.
Being overweight often causes the development of Type-2 diabetes, causing leg and foot pain. Older people who do not attempt to control their condition can even lose sensation and feeling in their legs and feet. This can lead to the development of small sores that can lead to serious infection.
Extra stress placed on the joints, tendons and muscles in the feet as a result of extra body weight may also cause heel spurs, or plantar fasciitis. Plantar fasciitis is an inflammation of the foot tissue, causing stiffness and pain when walking and climbing stairs. This can usually be relieved by foot stretches and custom made orthotic shoe-inserts.
Problems in the feet triggered by obesity can be treated by paying special attention to footwear. Proper support shoes that allow for good circulation, especially in the arch and ankle, are vital. A podiatrist can help you find what sort of shoe is most suitable for your feet. They can also measure you for special orthotics if necessary.
It could also be high time to start losing weight in order to treat and prevent diabetes as well as other life threatening diseases. Some methods include yoga and water aerobics, which benefit your entire body without placing stress on your feet. Don’t risk losing your feet by losing interest in them. Take care of your feet and your body, as they deserve the very best.
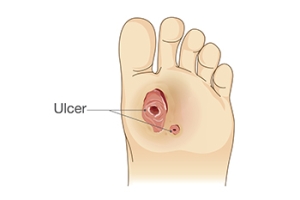
Diabetic Foot Ulcers Is a Condition You Cannot Ignore
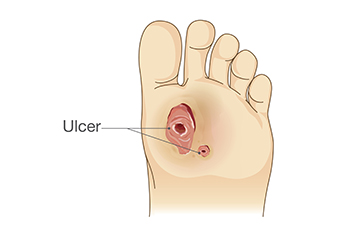
Nearly one in three people with diabetes will develop a diabetic foot ulcer, a slow-healing wound that can turn serious fast. These ulcers often start small, maybe like a blister or callus, but with poor circulation and nerve damage, they can quickly worsen without pain as a warning sign. Left untreated, infections can spread, sometimes leading to hospitalization or even limb loss. Prevention is key. Daily foot checks, wearing proper footwear, and keeping blood sugar in check reduce risks. But if you have diabetes and you notice redness, swelling, or a wound that is not healing, it is strongly suggested that you see a podiatrist for care as quickly as possible.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Patricia Mcilrath, DPM from Health One Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our offices located in Reading and Rittenhouse, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.